In popular culture, many women think of Kegels as exercises they can do to improve their sex lives. In reality, there’s not a whole lot of strong evidence that Kegel exercises improve sexual function. As a pelvic floor physical therapist and board certified orthopedic clinical specialist, I’m here to share some of my expertise with you about Kegels, and when they are – and aren’t – helpful.
Before we delve into this hot button topic, let’s have a brief history lesson on the “origin” of the Kegel exercise. Arnold Kegel was a gynecologist in the mid 1900’s who coined the term after observing that the pelvic floor muscles were weakened during the trauma of childbirth. He created a machine called the Kegel perineometer that could effectively measure the strength of the pelvic floor muscles for women having urinary and/or fecal incontinence issues. Biofeedback techniques, used in pelvic floor physical therapy today, also measure the strength of the pelvic floor muscles. I’m not really sure why it took a man in the 1950’s coining the term after his last name for these exercises to catch on, but boy did they!
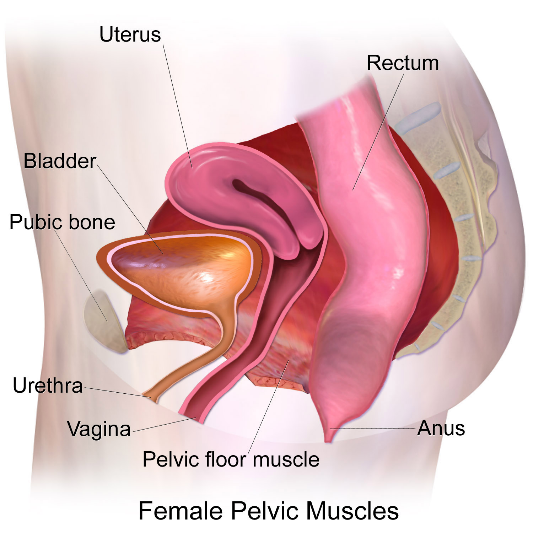
Fast forward to present day and the science about Kegeling hasn’t advanced much—hence the question: to Kegel or not to Kegel? The Kegel muscles—or in medical terms the levator ani muscles—are a group of muscles that make up your pelvic floor. They go from your pubic bone and sling around your anus and help control the opening and closing of your urethra, vagina, and anus. They have other important roles, too, but I’ll leave that for a later time. Weakness in these muscles can lead to things like incontinence: in other words, accidental leakage of urine, stool, or gas. (For the record, a person with a penis has these muscles too, but we are talking about the person with a vagina right now. )
Squeezing or contracting these muscles can help reduce incontinence symptoms, but these exercises aren’t for everyone. Some people have pelvic floor issues that can be made worse by Kegels or pelvic floor squeezes.
When can Kegels make the problem worse?
These exercises are probably not right for you if you experience any pain with vaginal intercourse, inserting a tampon, or speculum exam (the device used at the gynecologist) or if you have difficulty emptying your bladder or strain when you move your bowels Some people hold stress in their pelvic floor, very similar to how we hold stress in our shoulders and neck. Others just don’t have good awareness of how to relax the muscles, and some have had trauma to the pelvic floor. All of these things can lead to having “increased tone,” or tightness, in the muscles, which can lead to pain. Some people describe the pain as burning, others as a deep ache, but pain is pain and you shouldn’t have any pain “down there.”
What can women do, if not Kegel?
If you have any of these symptoms, along with incontinence, make sure you tell your physician. There are treatment options!
One treatment for these symptoms is pelvic floor physical therapy (sometimes called “women’s health physical therapy”). Pelvic floor physical therapy helps to correct pelvic floor muscle dysfunction which can contribute to pain with sex in addition to bladder and bowel symptoms. Pelvic floor physical therapists can work with you on different techniques (that aren’t Kegels) to address your particular symptoms. Kegel’s are typically used when the pelvic floor is weak and loose. But the pelvic floor can also be weak and tight. Kegel’s are not the right exercise when there is pelvic floor muscle tightness.
What are the circumstances in which Kegels can be helpful?
Now let’s talk about those of you who could benefit from doing pelvic floor contraction exercises on a regular basis. If you tend to lose some urine when you sneeze, jump, run, cough or laugh and don’t have any of the other symptoms I mentioned above, you can try some pelvic floor muscle squeezes.
One disclaimer with all of these instructions, please don’t practice this while sitting on the toilet. This can lead to not being able to fully empty your bladder and we don’t want that! This can lead to things like urinary tract infections (“UTIs”) and bladder infections.
To do pelvic floor muscle squeezes, breathe in and, then, as you breathe out, gently try and squeeze and lift those muscles – think about how you might squeeze when you’re trying to hold back gas or stop a stream of urine. Try about 20-30 gentle contractions throughout the day and vary the length you hold them anywhere from 2 seconds to 8-10 secs. Do you ever have those “gotta go RIGHT NOW” symptoms? This is called urgency. If you experience this you can also try and do 4-5 of these pelvic floor contractions when the symptoms occur. These squeezes can calm the symptoms down so you can walk rather than run to the nearest toilet. Research also shows that about half of people don’t actually achieve an appropriate pelvic floor contraction when they are told once or given a handout on what to do. Pelvic floor physical therapy can also help you understand exactly what you need to be doing.
So let’s summarize:
- Kegel was a dude who decided to coin a term that people with vaginas use today for our bodies, but a lot of women do Kegels without knowing details about how they might impact the pelvic floor. Let’s change that!
- Pelvic floor muscle contractions can help if you have urinary/ stool/gas? incontinence. 20 -30 gentle contractions throughout the day can be enough to help reduce symptoms.
- If you have pain/tightness in your pelvic floor muscles or struggle to fully empty your bladder, pelvic floor squeezing or contraction exercises probably aren’t the right thing for. Let your gynecologist, nurse or other clinician know!
- “Vagercising” (I think I coined this term?) can be satisfying if it is done right. Know what your pelvic floor needs before you begin.
To learn more about pelvic physical therapy, check out our videos here.
Do you have questions or comments about Kegeling? Write us at info@womanlab.org or on Facebook or Twitter with your questions.
Photo via Wikimedia Commons
Edited by Chenab Navalkha