For many of us, getting a good night of rest feels like an elusive pleasure reserved for fairy tale characters like Sleeping Beauty. Like eating well, exercising, and staying hydrated, we all know we should value sleep. And yet sleep often gets pushed to the backburner–a lofty goal for some, a seemingly impossible reality for most. But why can’t we bring the same sense of self-care to our sleep that we do to other parts of our lives? Personally, after researching the benefits of sleep hygiene for this article, I’d like to offer an impassioned plea for taking sleep seriously.
So let’s get into it. How much sleep do we really need?
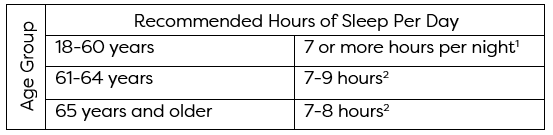
The Centers for Disease Control and Prevention (CDC) recommend the following hours of sleep per day by age group based on research from the National Sleep Foundation and the American Academy of Sleep Medicine. They even crafted this handy table below to illustrate the data!
When I look at this table a get a little knot in my stomach. On the rare occasion that I do find 8 hours to reserve for sleep, often I find myself tossing and turning with the anxieties of tomorrow on my mind and willing myself towards dreamland—counting sheep, listening to a white noise machine and hanging blackout curtains from my windows.
If you are like me, and fear you are on the short side of getting the recommended hours of sleep per night, you are not alone. According to data from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS), in 2022, 36.8% of adults in the United States report getting less than 7 hours of sleep per night. Results of the same poll found a relationship between sleep and well-being. Apart from itchy red eyes and a grumpy disposition, lack of adequate sleep can take a serious toll on our bodies both mentally and physically.
Sleep disturbance is especially common among women with cancer. In fact, the Clinical Handbook of Insomnia reports that sleep disturbance affects between 30-50% of cancer survivors. Sleep disturbance during and after cancer can occur for a variety of reasons including emotional distress, and as a side effect of chemotherapy and radiation. Ironically, increased fatigue during the day can lead to mild insomnia at night, since spending the day napping can preempt a restful night. Sleep disturbance disproportionately affects female patients with breast cancer (80%) and patients actively receiving chemotherapy (60-80%). Am I preaching to the choir?
Sleep can affect your sex life.
Anecdotally, our patients tell us that improving sleep can help improve sexual function issues. But here at WomanLab we are glasses wearing, PubMed scrolling research scientists (and proud of it!). These patient anecdotes led me to my own question—what does the scientific literature have to say about sleep and sexual function in women?
This won’t come as a surprise, but the majority of clinical research on sleep and sexual dysfunction has focused on men and erectile dysfunction. While we care about men here at WomanLab, we believe that the sexual function of women deserves the same level of scientific inquiry as everyone else.
While scientific evidence in this area is lackluster at best, researchers are starting to pay attention to the relationship between sexual function and sleep in women.
A longitudinal pilot study of 171 women published in the Journal of Sex Medicine in 2015 reported that women who reported longer sleep duration were more likely to engage in partnered sexual activity and greater next-day sexual desire. With only a sample of 171 women it is difficult to suggest that these findings apply to ALL women, and we shouldn’t, but it’s a pretty strong clue that there might be a relationship between sleep and sex.
Another, more recent and rigorous study in the journal Menopause in 2017 found an association between shorter sleep duration, higher insomnia scores, and decreased sexual function in a HUGE sample of postmenopausal women (93,668 women to be exact) from data collected in the Women’s Health Initiative Observational Study. It makes sense that this study was published in Menopause: many women experience disruptions to their sleep quality during the menopause transition. Researchers haven’t been able to parse out whether women experience difficulty sleeping as a direct cause of menopause, or whether this sleep disruption is caused by other symptoms (think, night sweats). The authors of this study stated the importance of quality sleep for sexual function and called for researchers to build increased evidence of this relationship with a longitudinal study of this relationship.
Most recently, a study in the journal Menopause in 2021 found an association between poor sleep quality and increased sexual dysfunction among a sample of 2,487 women from the Data Registry on Experiences of Aging, Menopause, and Sexuality (DREAMS). This study differs from the others mentioned in that it is the only one to measure the effect of sleep quality (how well you sleep) on sexual function, rather than sleep duration (how long you sleep). Interestingly, the study also measured sleep duration and did not find an association between shorter duration and sexual dysfunction, a finding that differs from previous studies. The authors state that the reason for this lack of association is unclear, but speculate that there may be unique mechanisms that are associated with poor sleep quality and not sleep duration that are responsible for the association of the former, but not the latter, with sexual dysfunction.
Further study in this area would help to better solidify our scientific understanding of the relationship between sleep quality and sexual function and the mechanisms of action that drive this relationship (i.e. what exactly about good sleep leads to good sex?). In other words, the jury is still out on whether the relationship between sleep and the sexual function of women is strongly backed by science, but the current scientific evidence is leaning towards a “yes.”
This blog is a reminder to consider sleep hygiene an essential part of self-care. But it is also a call to action for research scientists to continue to study the relationship between sleep and sexual function in women with cancer. Why? The more tools we can keep in our back pocket to use in the recovery of sexual function before, during and after cancer treatment the better.
Now that we know how much sleep we need, how important sleep is to our quality of life (especially for cancer patients) and what research currently exists on the relationship between sleep quality and sexual function, stay tuned for Part 2 of our sleep series where you will learn about evidence-based ways to improve your sleep!
- Watson NF, Badr MS, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015; 38(6):833-834.
- Hirshkowitz M, Whiton K, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43.
Edited by Leilani Douglas
Updated September 3, 2025 By Delaney Romanchick, Lisa Medalie PsyD, RPSGT, DBSM, and Stacy Lindau MD, MAPP