Incontinence (or peeing when you don’t want to) is one of those things that’s in the category of “my mom never told me that!?” It’s mostly unexpected, embarrassing, and—quite frankly—not really talked about enough.
I remember the first time it happened to me was after delivering my lovely daughter. I must have had a full bladder, laughed, and then… just wet myself. I remember talking to my husband and stopping mid-sentence, “Uhhh… I’m wet and not in a good way!” My immediate next thought was, “Damn!!! I wasn’t prepared for this!” What followed were swirling thoughts (pun-intended) of, “I’m getting old.” “Will I smell?” “Will I be featured in one of those commercials for adult diapers?” and, of course, “I’m never having another kid again.”
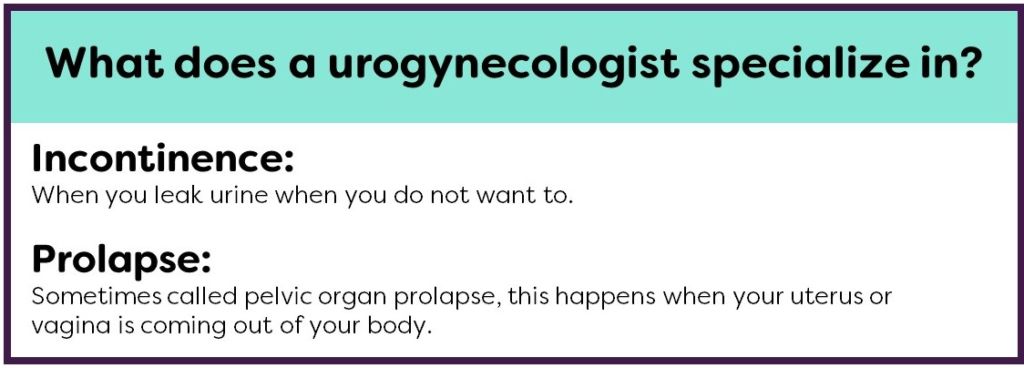
Here’s the thing—I had these thoughts and I’m a urogynecologist. In other words, even as a gynecologist who specializes in treating women with incontinence and prolapse, my own incontinence took me by surprise. The good and bad news is that you’re not alone if this happens to you. By estimates, almost 50% of women have some incontinence, and only some seek treatment for it (1). There are different types of incontinence, and there is help for it if you’d like. It can be an embarrassing thing to talk about, but if you ask around you’ll see you truly are not alone and other women will likely want to know what you find out too. If you can’t find a urogynecologist near you, there are many gynecologists and urologists who also treat women with incontinence.
 In this post we’ll discuss the different types of incontinence, how and why it happens, and in Part 2, we will talk about what you can do about it. We won’t discuss adult diaper brands (the cheapest!) or why they’re so expensive (no idea) because my main goal is you not wearing them, if you don’t want to!
In this post we’ll discuss the different types of incontinence, how and why it happens, and in Part 2, we will talk about what you can do about it. We won’t discuss adult diaper brands (the cheapest!) or why they’re so expensive (no idea) because my main goal is you not wearing them, if you don’t want to!
1.What are the different types of incontinence?
There are 2 main types of urinary incontinence (pee): Stress and urge.
- Stress incontinence is peeing on yourself when you laugh, cough, sneeze, or exercise. This is the, “I laughed so hard I wet my pants” kind of incontinence. And it’s the one everyone talks about. Mostly you can predict when it’s going to happen and try to do a Kegel (hold it in using your pelvic floor muscles) to prevent it.
- Urge incontinence is when you dribble or full on wet yourself as you’re rushing to the bathroom. For a lot of women this starts with having to go to the bathroom a lot and feeling like you have to go right back after you’ve already been there. This is the, “mom’s in the bathroom again” kind of urge and is called Overactive Bladder Syndrome. My mom is a great example of this. She has such frequent urges she knows where all the bathrooms are and their specifics- which ones are cleaner, which ones have lotion, which ones have the best paper towels (you catch my drift). When this gets worse, you can start to leak (or more) on the way to the bathroom. The downside of this is that it can start to limit when you go out of your house, on dates, and go anywhere where you don’t know if you’ll have a bathroom. This can lead to feeling isolated and staying away from friends. Sometimes it starts as you pull into the garage or when your hand is on the bathroom door handle: “key in the door syndrome” we doctors like to call it. In other words, you have an URGE.
Then there are the times when you leak when you’re having sex. This could be either stress (from a penis or a toy rubbing on the urethra, which is the tube from the bladder to the outside) or urge (usually at the time of orgasm from your bladder contracting). It’s sometimes difficult to tell if being wet is from excitement or urine. If you’re wet with excitement, then that’s great, and you shouldn’t shy away from sex. This is sometimes called female ejaculation or “squirting.” Really, no one likes to talk about this one, but it definitely happens more than anyone lets on. Depending how and when (with orgasm or not) it happens we treat it differently. Sometimes just the thought that you may leak with sex, or in general, and may smell of urine at times stops women from trying to be intimate. Don’t fear! You’re not alone and likely don’t smell! Studies report that up to 45% of women avoid intimacy due to incontinence (2, 3). There are treatments as well to get you back to feeling sexy and wanting to be intimate.
There are a lot of changes your body goes through during pregnancy, during delivery, right after, and a long time after! We know that being pregnant at all, and having a vaginal delivery, increase your risk for both types of incontinence- stress and urge (4). That being said, even women who were never pregnant have incontinence too.
Then there are also a few special circumstances- after pelvic surgery or pelvic radiation for a gynecological cancer. Surgery and radiation have their own problems and can lead to both stress and urge incontinence. Sometimes the urethra is so weak or scarred after radiation that urine just leaks out, like an open hose. If this is you, there is help, you are NOT alone, and you should definitely see a specialist!
2. How did this happen to me?
I wish we had a crystal ball and could predict if and who this is going to happen to, but we don’t… not yet, at least. It’s easier to divide the reasons based on the type of incontinence- stress or urge.
With stress incontinence, the problem starts with a weak urethra and a loss of support from the tough tissue in your vagina that supports your urethra. Most of the time this is from having babies. It tends to be more common when you have a vaginal delivery, but happens from just being pregnant too. The pressure and damage from delivery damages the support to the urethra, so the urethra moves more. I know you’re thinking right now, “If I would’ve known….” But the truth is we don’t have a good alternative because cesarean sections have their own problems. Even if you’ve never been pregnant, we know other things can lead to stress incontinence too. Heavy weight, loss of estrogen after menopause, and just getting older leads to weaker urethral support, so stress incontinence can happen to anyone.
Urge incontinence, leaking as you’re running to the bathroom, is really a nerve problem. This is when the nerves from your bladder to your brain that control how and when you pee are damaged. In an ideal world, your bladder could sense when it was full and would send a message to your brain. Your brain would then figure out if it’s a good time to pee (okay = near a bathroom; NOT okay= driving), and then tell your bladder. If it’s not a good time, your bladder would relax and your pelvic floor muscles contract and you could hold it. If it was okay, then your bladder would contract and your pelvic floor muscles would relax so you could pee. When you have nerve damage, your bladder has a harder time sensing when it’s full, and can sometimes contract when you don’t want it to making you pee before you’re ready. This means that your bladder gets the signal to go before you’re ready making you feel like you need to pee more often than you used to. In addition, when the bladder contracts it can lead to bladder emptying- or peeing- before you’re ready.
Ok, so that might have been a lot of information. You might now be wondering what you can do about it, what treatments are out there, and if you’re stuck with incontinence (spoiler alert: you’re not!). Part 2 is coming up.
You can always reach us at info@womanlab.org. Have a story about incontinence you think everyone can relate to? Tweet us at @WomanLab.
References
- Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. The iceberg of health care utilization in women with urinary incontinence. Int Urogynecol J. 2012;23(8):1087. Epub 2012 Apr 12.
- Rogers GR, Villarreal A, Kammerer-Doak D, Qualls C. Sexual function in women with and without urinary incontinence and/or pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(6):361.
- Hilton P. Urinary incontinence during sexual intercourse: a common, but rarely volunteered, symptom. Br J Obstet Gynaecol. 1988 Apr;95(4):377-81.
- Patel DA, Xu X, Thomason AD, Ransom SB, Ivy JS, DeLancey JO. Childbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol. 2006;195(1):23. Epub 2006 Mar 30.
Edited by Megan DePumpo and Danielle Grubb
Photo by Frank Busch via Unsplash