“I remember when I used to play with my hair… back when I had hair.” My hand dropped. My heart sunk. “I am so sorry. Bad habit,” I offered the patient sitting beside me in the overly lit gynecologic exam room, as I finished tucking hair behind my ear. Her first appointment in the Program in Integrative Sexual Medicine (PRISM) Clinic was concluding and we now had a few minutes alone for me, as a newly trained patient educator, to provide her with basic, non-medical information to aide in optimizing her sexual function.
She had hair – it was just short and I certainly would have been more aware of my behavior if she were experiencing drug-induced alopecia of the scalp, I told myself in an attempt to rationalize my actions. I was so focused on saying the “right” thing that I failed to consider how what I was doing might make her feel. Any Hollywood production or pharmaceutical advertisement will emphatically remind you that bald=cancer and hair loss can reliably be found on the list of common side effects provided to a patient presenting for chemotherapy infusion. However, when it comes to sexual function, women diagnosed with cancer rarely receive anticipatory guidance on what changes to expect to this vital aspect of her life.
As a patient educator in the PRISM Clinic, I’ve interacted with more than 200 women affected by cancer. Some of these women are in the acute phase of treatment, receiving chemotherapy or radiation, or recovering from surgery. Many others are post-treatment and navigating the sometimes complicated world of survivorship. They may have been suffering from the sexual consequences of their life-saving treatments for years (at times, decades) without relief.
While her hair may have grown back (though not always fully in the less visible regions of the body), much of a cancer survivor’s pain and suffering may not be visible to the eye.
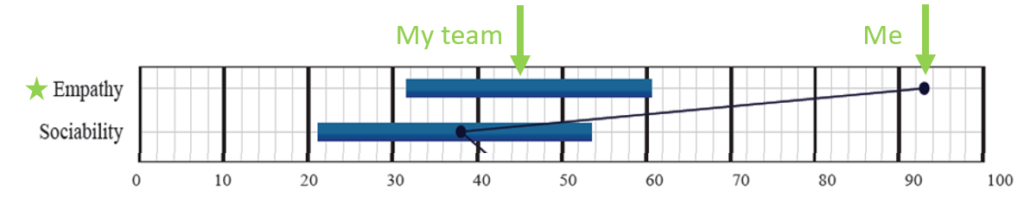
What could I, a 20-something woman with no history of cancer offer this 60-something woman? How could I possibly understand the challenges she had endured to her intimate life? What could I say to show that I cared? I certainly have a high propensity for empathy (see below image), but could I truly practice empathy and serve as a trusted partner in this woman’s path to recovery? It was this self-doubt, I believe, that culminated in the hand-to-hair impulse.
The truth is – I did have something to offer. I had extensive training and education to prepare me for the position. I had evidence-based information and resources in the form of patient education materials to address low libido, painful intercourse and other sexual concerns. I knew how to locate a sex therapist in her neighborhood and what she could expect at her first visit and which local sex shops carry graded vaginal dilators*. I could tell her where to find a vaginal moisturizer at the drugstore and how to use it. I had tips from the experiences of the patients that had come before her – including suggestions for a fun date night in the city or a helpful book to read. I had a team of female scientists prepared to research the questions without clear answers.
And while my delivery had room for improvement, I had the determination to ensure she knew that we were in this together.
The basic self-care information I share with women presenting for clinical care is drawn from the best available science as well as the insights and experiences from real women discovering what works. WomanLab is a place to spread this knowledge beyond the woman-to-woman patient education session so that all women and those who love women can access sexual self-care recommendations.
Two years and countless patient education sessions later, I’ve learned that the “right” words can be difficult to find but “you are not alone” is a pretty good place to start.
* See section “Using dilators for vaginal tightness” within link.
Edited by Chenab Navalkha
Updated June 2, 2025 by Delaney Romanchick